In the past 2+ years in the US, the medical industry has been through a draining and dramatic strain due to the COVID-19 pandemic. Doctors and nurses were overworked, lauded as heroes, were at the center of both praise and criticism due to COVID and COVID-deniers, and have faced incredible and unprecedented struggles. So, in no way do I mean to disparage the medical field. Doctors and nurses are a vital necessity for the health and wellness of our society at large. The incredible amount of knowledge, training, tuition money, grueling residencies, and other parts of being a physician, surgeon, nurse, nurse practitioner, pharmacist, or hospital employee inspire a lot of awe. However, as a woman and as a school leader, I have to say that a profession that claims to be based on “doing what’s best for patients”, often falls very short in not only it’s overall treatment of women (especially minority women), but an important subset of women – educators.
On paper, medical doctors and educators have a lot in common. Both are professions that are actually made up of a MAJORITY of women. Both professions are filled with women with advanced degrees who face a pay gap between themselves and their male colleagues (especially when those women are women of color). However, the difference in the amount of public respect, pay, and the ability to maintain a work-life balance are often vast. While many nurses and doctors at hospitals work grueling shifts, they don’t often take tremendous amounts of work home with them. Growing up, I watched my mother become an award-winning nurse at the University of Chicago. She’s won every nursing award that the hospital gives. She has an incredible work ethic and was intensely devoted to her work, her patients, their families, and her coworkers for her entire career. That being said, as a full-time nurse that earned generous overtime pay on holidays or for staying late, she never once took a piece of paperwork home. She worked 3, 12-hour shifts per week plus every-other weekend. She earned a great living, had a good work-life balance, and when she was home, she was HOME. The lifesaving, incredibly brilliant trauma-surgeon that saved my ex-husband’s arm from amputation works 2, 16-hour shifts a week (which might be extended due to complex surgeries), and every-other weekend (plus being on-call while other surgeons are on vacation/out of the office, etc.) Of course, both of these examples are anecdotal and were HOSPITAL employees at the busy University of Chicago Hospital – not private practice or local doctors’ offices. The vast majority of my current frustration with the medical industry is actually NOT with hospitals in general, but rather with local medical offices.
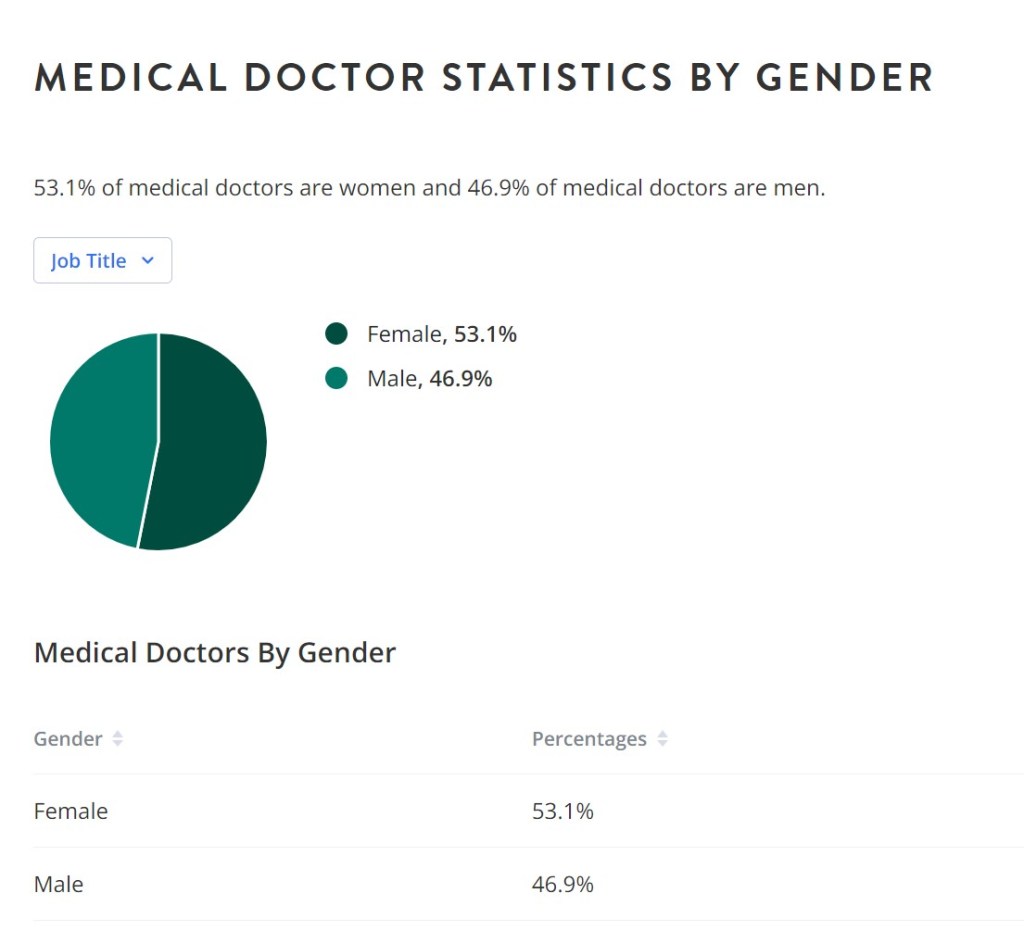
But before we get into all of that – let’s look at some demographic data of these female-majority professions. According to the research on www.zippia.com, regarding medical doctors in the United States, 53% are female with average pay varying per region between $120k and $192k (see graphics below). Obviously, those with additional degrees, more specialized areas of expertise, etc. could exceed this amount. Additionally, a report by The Physician’s Foundation released in 2018 found that a majority of doctors worked 51-60 hours per week (see graphic below).
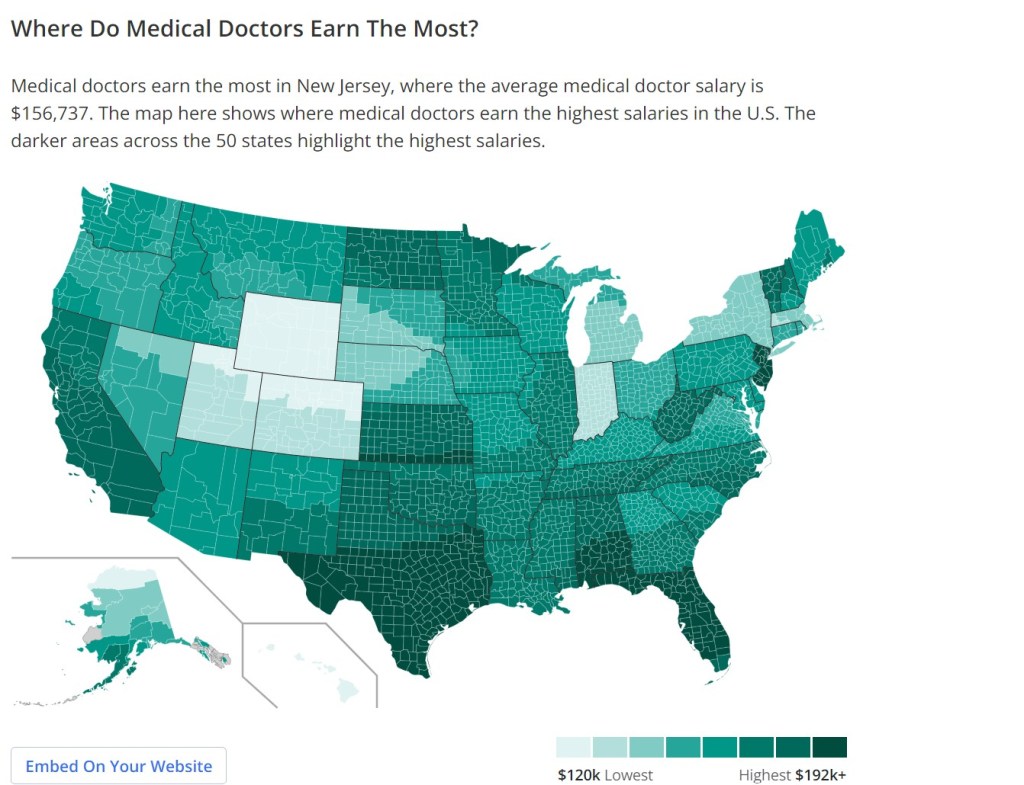
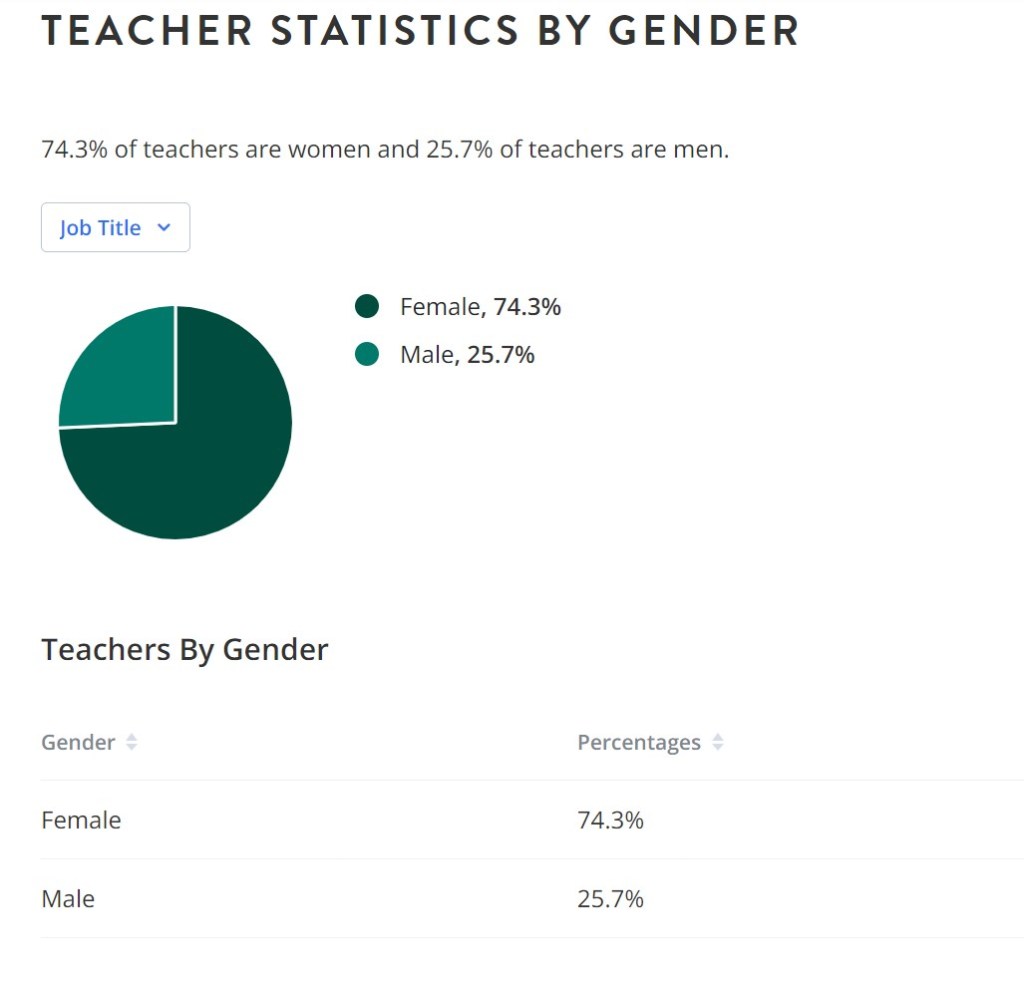
Let’s compare this same information for teachers (ALSO a highly educated, majority-women profession that has a pay differential between males and females). Teachers are 74% female, with an average salary (depending upon region) between $31k-$63+k (see graphic below), and per recent research published in Education Week, the average teacher works about 54 hours per week (read the full article on how teachers’ workweeks break down here). What a STARK difference in pay for somewhat similar hours. (And these statistics do NOT include the piles of paperwork that any of these educators take home and work on on their own time).

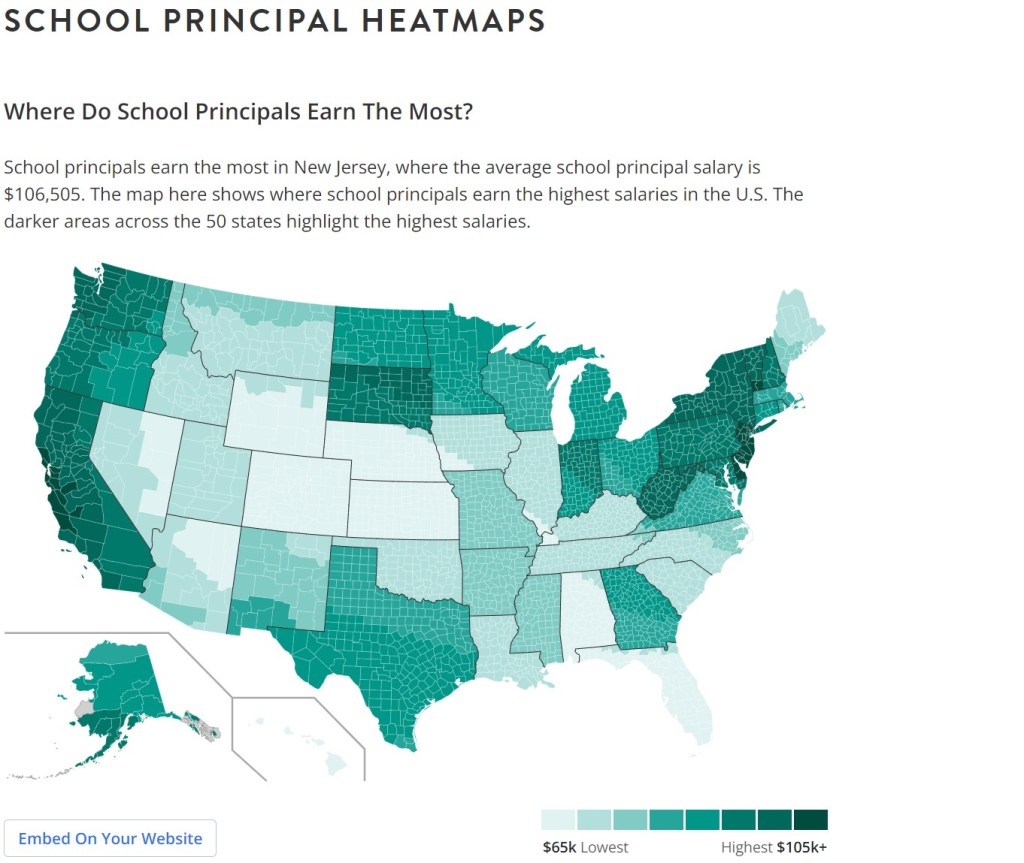
Ok, ok – maybe comparing medical doctors to teachers isn’t really fair. After all, aren’t medical doctors required to have much more education, training, and experience than the average classroom teacher? So, let’s talk about school principals. ALSO, a female-dominated field (but only if you lump all schools together though. A VAST majority of high schools are led by men and since there are many more elementary schools and the majority of THOSE are led by women it sort of skews the data). Female school principals account for 55% of all school principals and make an average (regional variations) of $65k-$105+k (see graphics below). Additionally, the average school principal reported working about 60 hours a week BEFORE the pandemic; but in my experience, a follow-up study with updated numbers just might show this being AT LEAST 60 hours a week.

Why do I bring any of this up at all? Well because I’m a woman who needs to see a gynecologist. And good luck doing that if you aren’t a woman who can go to the doctor between 9 am and 3 pm. Recently, I (tried to) make an appointment with my gynecologist. She only works between 9 am and 3 pm. So, an early morning OR an afternoon appointment would mean that I would have to take off of work (since I can’t go for a 7 am appointment and just come in a bit late OR leave with the students at 3:15 for a 4 pm appointment as neither of those are options). Even taking a half-day isn’t possible unless I can get guaranteed an on-time appointment at 10 am and get to my building by 11:30; or get a guaranteed appointment between 12:30 and 2:30 so I can stay until 11:30 (the cutoff time for “half-day).
Being the educator that I am – I don’t like to take time off when students are in the building. Although it’s less of a big deal now that I’m an administrator – it’s still not ideal. I remember the pressure (some put on myself by myself and some put on me by students, parents, and administrators) to not take off of work. “We only have 180 days with students – everyday counts”, “not enough learning happens when there’s a sub”, “it impacts the whole building when an adult is out”. And all of those things are true. So, like MANY educators, I RELY on early-morning, late-afternoon, weekend, or evening appointments. Failing those options, I pack my Thanksgiving, winter, spring, and summer breaks chock full of eye doctor, annual physical, gynecologist, blood test, mammogram, and dental appointments. Frankly, it sucks, and I’ve always resented having to line up tons of appointments on the rare days off of work that I get all to myself. I’ve always preferred the early-morning, late afternoon, or weekend appointments so that I don’t NEED to give up vacation time, impact my students, or burden my coworkers so that I can sit in waiting rooms. However, this has become less and less of an option for me lately. Every time I call an office to try to get an early, late, or weekend appointment I am told, “oh the doctor no longer has any evening, weekend, or early morning hours”. So begrudgingly, I mentally prepare myself to give up Winter, Spring, or Summer break days. And lo and behold, apparently all the doctors are also taking off during all of the school breaks as well so they can hang out with their own children. And I GET IT. I understand the desire to take a family vacation, spend time with family, etc. But those same doctors ALSO have a certain expectation that their own children will have teachers on a daily basis when they go to school. They have a certain expectation that Open Houses, Back to School Bashes, Parent-Teacher Conferences, School Tours, and Meet the Teacher Nights will take place outside of those teachers’ and administrators’ paid hours. So why don’t those same doctors have the occasional night, weekend, late afternoon, or “around the holidays” hours? Don’t the women who care for doctors’ children deserve the same convenience that their children’s teachers give to them?
I am ALL FOR work-life balance. And I am not suggesting that any overworked and stressed out medical professional works MORE hours themselves. I am asking why more of them won’t work SMARTER? For example, even if the cost is a little higher, I will remain an avid patient at my dentist’s office until the end of time. They are closed every Monday and open at noon every Tuesday. They are open Tuesdays from noon-8pm and Wednesdays-Fridays from 8-4PM and every other Saturday from 7am-noon. The 4 dentists take turns on who works on Saturdays and Tuesday evenings so that they each only work 1 in every 4 evenings or Saturdays. As a result, I never have to take off of work to take care of my dental health. This includes their endodontist! I have had 2 root canals at 6 PM and haven’t had to take off of work. It meant that my students, my teachers, and the other administrators in my building didn’t have to feel my absence and I also remained healthy enough to keep working because the dental issue was taken care of before it turned into an infection.
How many average workers (teachers or otherwise) want to take off of work on a random Tuesday morning to get a physical or an eye doctor appointment? (Especially if you get paid by the hour and will lose income?) Survey your patients to see what times would be the most convenient for them and eliminate the times/days that are less popular and maybe close on Monday and Tuesday but work Wednesday evenings and Saturday mornings. Split up those days with the other doctors in your office/network. I guarantee all of the shift workers and teachers and school administrators that can’t take off of work on a Wednesday at 1 PM would be grateful. A person that is willing and able to receive preventative or basic care at a convenient time would be a loyal patient. Regular, everyday medical care is what prevents more serious illness and keeps people healthy. Imagine the long-term impacts on children whose teachers have medical issues that aren’t diagnosed early and result in a leave-of-absence? When I asked the receptionist at my gynecologist’s office what I could do if I had a serious medical concern and they couldn’t get me a first-thing-in-the-morning appointment, her response was “I dunno, go to the emergency room, I guess. We tell people to just take off of work.” I was so annoyed that I looked for another doctor and when I called his office was told that there was a 4-month waiting list for new patient appointments. Imagine the uproar from doctors (or any parents) if schools said, “sorry but we only do parent-teacher conferences from 9-3 and we don’t have events like Open House outside of the school day – just take off of work.”
If there is one thing that the COVID-19 pandemic has done to transform the world of work, it was adding flexibility to the workplace. Many industries are allowing for flexible hours, working from home, hybrid work, or a combination of all of the above. Even the medical industry has embraced the teledoc system for more minor medical conditions that don’t require testing or in-person interaction. Many of the “essential workers” such as retail workers, school employees, many medical employees, and those involved in the transportation industry haven’t gained any of this flexibility or the option to work from home or split our hours. As a result, educators still have to make the difficult call of, “should I leave my students today and impact their education to get a pap smear/blood test/cancer screening from a doctor that won’t work before or after school, on the weekend, or during school breaks?” or “Should I just put it off?” Either way – those doctors’ (and other people’s children) will be impacted. Either the teacher will miss a day, or they might actually get ill and miss potentially a lot more days, or worst-case scenario they’ll have to have a long-term sub due to a serious illness or even death). Meanwhile, those same doctors and parents expect those educators to be present outside of their contracted hours to support them and their children through athletic games, Open Houses, conferences, parades, events, Science Fairs, etc. We can talk all day about “self-care” and how if you have the PTO that you should take it when you need it – but educators will ALWAYS have the added pressure of how this will impact the learning of their students. Many are more than willing to take care of their personal business on their personal time – but they can’t find doctors that will accommodate them. So, doctors, I beg you to take your children’s teachers, principals, paraprofessionals, and other school staff (as well as essential workers in other industries that don’t have flexibility) into your planning of your office hours and operational systems. No one is asking you to work more, just work differently. Consider the health of the people that care for your children and how your children might be impacted by missing their teacher (who is willing to come and see you at 4 PM or on Saturday morning with no impact on your child’s education).
Women’s health in general in this country is in a sad state of affairs. There simply aren’t enough OB/GYN’s and in my anecdotal experience, the quality of a lot of the gynecologists that myself and the women in my life have come across have left a lot to be desired. I don’t have data to back this up – it’s just a feeling that I’ve developed over the years; but a lot of gynecologists don’t seem all that interested in women’s actual health. MANY of them love babies, pregnancy, pregnant women, and helping women give birth. It’s not only obvious by the decorations in their office, their excitement when a pregnant woman walks through their doors, but it also shows in what kind of care that their office hours show has value. Once I FINALLY got an appointment at the gynecologist (2 months AFTER I was due to go AND had to take off of work), I was at the counter paying my co-pay and waiting for the receipt to be handed to me. While I was standing there, I overheard the other secretary get a phone call from a newly pregnant mom who was calling to make an appointment. She was fit in THAT WEEK with no notice. But when I had called with a serious MEDICAL CONCERN it took me 2 months to get that same courtesy of an appointment. (Because the doctor only blocks out 2 hours a day between 10-12 for non-pregnancy related appointments). If this had been a one-time thing, then maybe I could consider it a fluke. But at the same gynecologist, 2-years prior (after my having to take off of work to have a procedure done due to the lack of early morning or late afternoon appointments), I was called AS I WAS PULLING INTO THE PARKING LOT to be told “the doctor is with a patient in labor at the hospital can you come back in 2 hours?” A procedure that I was having to TRY TO PREVENT cancer. To add insult to injury, the procedure wasn’t successful, and I needed it repeated. Again, I took time OFF OF WORK to come in for the re-do when it was convenient for the doctor. 2 days before the procedure the doctor’s office called me to tell me “The doctor has to reschedule you’ll need to come in on the 10th instead.” In a total Karen moment, I told the secretary that that would be impossible as I’d already taken the time off – whomever was covering for the doctor when her patients went into labor would have to do the procedure. She informed me “she doesn’t have anyone to cover. All the appointments just need to be rescheduled. The other doctors in this office have their own appointments scheduled already.” (So do all of the teachers that I have to pull from their breaks to cover the classes that have no sub, and we make it work even though it’s not even a little bit ideal). I was so nervous and worried that I cried on the phone. She took pity on me and told me if I promised to be in 25 minutes earlier than I’d originally planned then the doctor would have enough time to do the procedure and go to the hospital for the C-section.
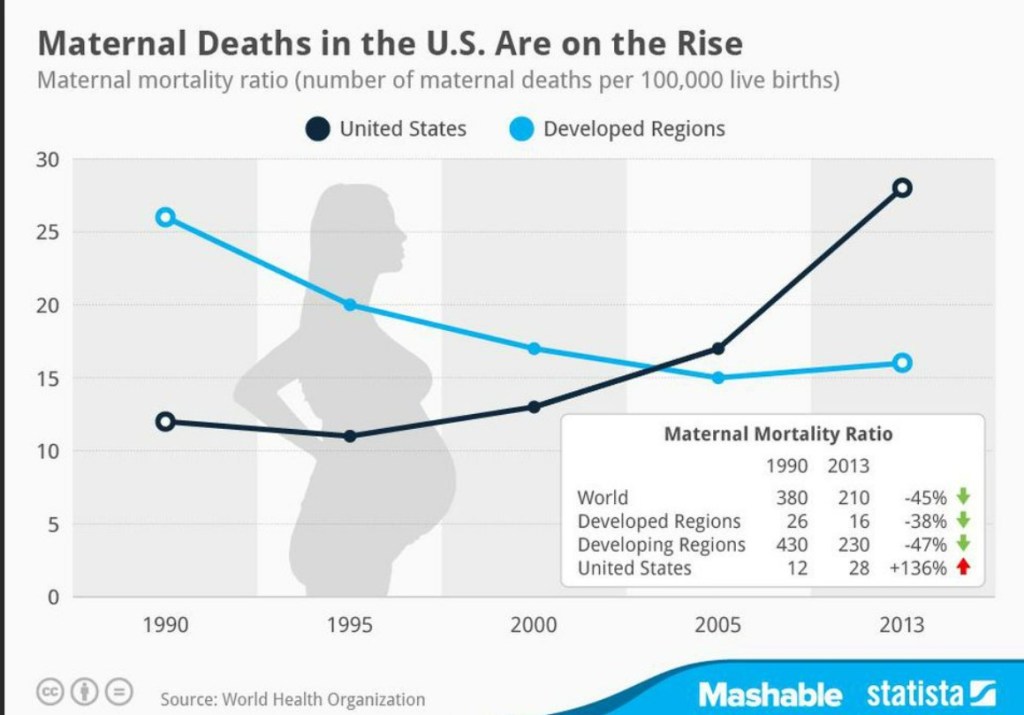
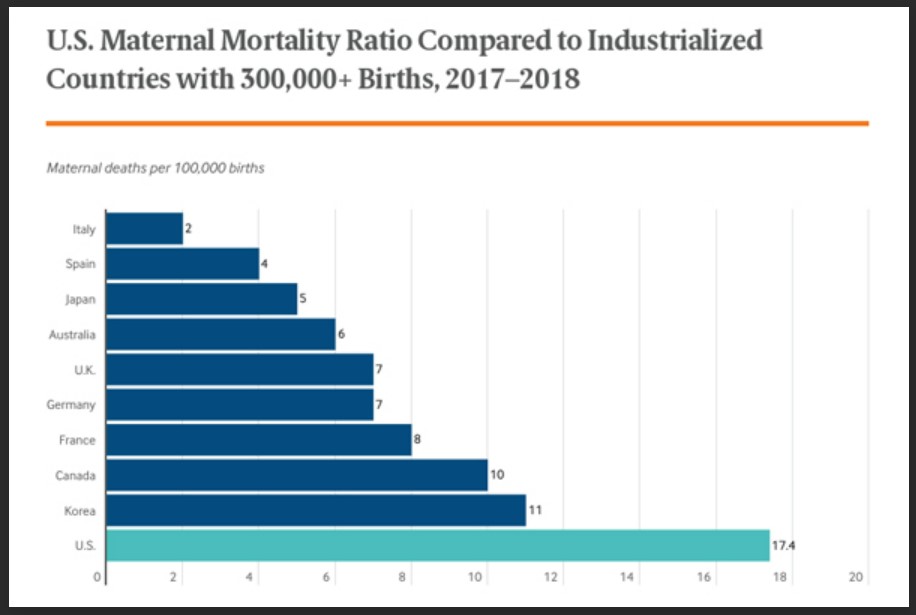
I 100% get it – babies come when they want to come. They don’t break their moms’ water between 9 and 5. They’re born when they’re born. But it’s not just while the moms are in labor has my care been de-prioritized. Many times, while in a gynecologists’ waiting room I’ve been made to wait while a pregnant mom-to-be gets to go first (even when my appointment time was first). In the past 4 years, despite having some serious gynecological issues, my gynecologist has spent maybe the equivalent of 45 minutes of her time with me in an exam room. Our appointments often feel rushed-through and are sometimes for painful procedures that are very stressful to undergo. Even when I have been there and there is an empty waiting room, these appointments seem to have been given less precedence than the pregnant patients’ routine appointments. I got so frustrated last year that I actually googled the phrase “how to find a gynecologist that doesn’t deliver babies and only deals with women’s health issues”. Needless to say, I didn’t have a TON of local results pop up. Many women in my life have had similar issues. IUD placements, birth control consultations, ovarian cysts, fibroids, cervical and ovarian cancer, and endometriosis are all health issues that women that I know have dealt with over the years. And their appointments/care are often on the “back burner” of their doctors’ rotation. You’d think that with all of this over-prioritization of appointments and care for American pregnant women that we’d have the best outcomes in the world. However, per a 2020 CDC report – that’s FAR from the truth.
The United States has one of the highest maternal mortality rates, if not the highest, in the developed world.
https://www.americanactionforum.org/insight/maternal-mortality-in-the-united-states/
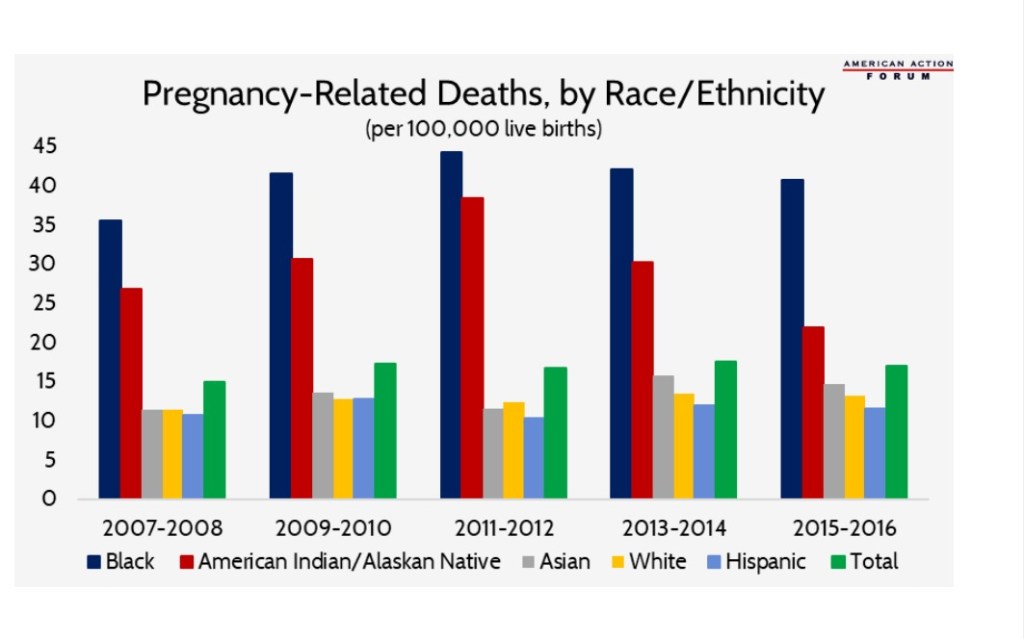
Of course, in the report it is even pointed out that there is disparity between white and minority women with minority women dying even more often than white women. As you can imagine the number of deaths increases as the woman’s insurance coverage amount declines. To put it in scary figures, it is safer for women to give birth in EVERY SINGLE OTHER FIRST WORLD COUNTRY on the planet – and most of the third world ones as well with the exception of Sub-Saharan Africa. And it’s getting WORSE not better. So, the “most important job” that American OB/GYN’s are “blowing off” other things for isn’t even going well. With the ridiculous new laws being passed with regulating women’s healthcare/birth control/abortion/miscarriages/forced birth/gender-affirming care can anyone predict anything more optimistic than “more deaths on the horizon”? If you were in medical school right now, would you choose a specialty under such a horrible microscope? Governed in some states by confusing and patient-harming laws? While we have a shortage of doctors now – what will happen when the ones that we do have (despite their range in skill levels) are vastly diminished?
My mom the nurse has always given people the advice to “get a second opinion they’re just doctors they’re not gods despite what their egos may lead you to believe.” I’ve given the same advice to people in my life before, but it wasn’t until my recent health issues that I truly listened and took it myself. After my marriage fell apart due to my husband’s cheating and stealing of massive amounts of money from me, I started having weird and painful abdominal pains. They felt like sharp menstrual cramps but were not near my period and were further up near the base of my ribs on my right side. I went to my general doctor, and she listened, examined me, and set me for a large battery of tests. I had abdominal ultrasounds, transvaginal ultrasounds, x-rays, a CT scan, and blood tests. When they all came back normal, the doctor referred me to a gynecologist to rule out things like endometriosis or fibroids or ovarian cysts (although she admitted that she didn’t see anything like that on my ultrasounds). So, I went to the gynecologist that she referred me to.
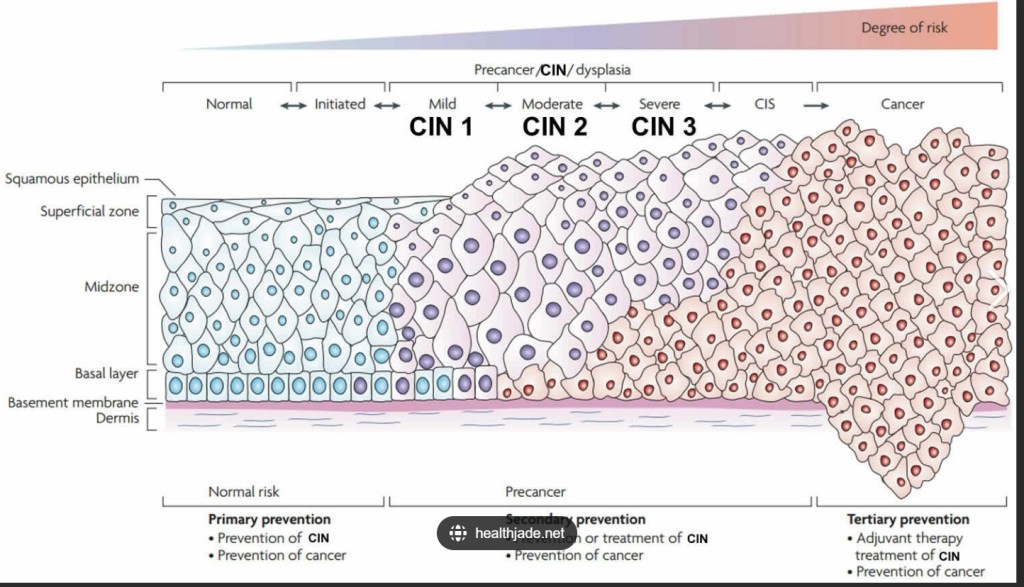
In retrospect, I should have stopped seeing this doctor after the first appointment. But I was still so shaken by what was going on in my personal life that I let things slide that I shouldn’t have. I told the doctor I needed testing for STDs since I’d been cheated on and that I had been having a lot of pain. She recommended that I go on birth control pills to control my cramps. I teared up and told her that I had stopped taking them because my husband and I had planned to try for a baby. I wasn’t even divorced yet and felt that taking birth control pills would not only mean that I was admitting to defeat; but was also potentially closing the door forever on what I had so desperately wanted. I told this to the doctor tearfully and her response was “well just so you know if you get pregnant at your age it’s dangerous for you and the baby anyway. I wouldn’t recommend it.” So, we did the exam, she told me to take some Midol if I got cramps, and I went out to the car and sobbed feeling like my concerns were sort of dismissed. The entire appointment minus all the waiting in the waiting room and in the exam-room waiting for the doctor to come in took maybe 20 minutes total, and I walked out feeling like I had no answers. A few days later my test results came back and thankfully I was negative for HIV, gonorrhea, syphilis, meningitis, herpes, and a whole host of other infections. Unfortunately, I tested positive for HPV – most likely due to my husband’s recently discovered serial cheating. The doctor had me come in for a colposcopy procedure to do a biopsy to ensure that the lesions weren’t cancerous or pre-cancerous. The procedure is not fun, and they don’t use any sort of pain medicine. That first test’s results were CIN1 – mild dysplasia that the doctor seemed unconcerned with and told me is a “mild concern” that as long as it doesn’t progress would most likely clear up on its own.
The second year, the process was repeated. She did another colposcopy, and again stated that there was little to worry about as her samples showed CIN1. I asked her if I should get the HPV vaccine as I had seen a commercial that it was now recommended for women up to 45 years of age (When it first came out, I couldn’t get it because I had just turned 22 and it was only given up to the age of 22). She told me that it would be a waste of time as I had already been infected and the vaccine would only prevent new infections. Most of my mysterious abdominal pains had stopped although I was having heavy bleeding and very bad cramps during my period. I told the doctor and again she told me that I should go on birth control pills. I told her that I was simply not comfortable closing that door as I had started dating and had come to terms with “if it’s meant to happen it’s meant to happen”. She again told me to take Midol if I had cramps.
The third year was this year. In February I went for my appointment optimistic that the infection had cleared (the doctor told me repeatedly that most people have cleared the infection by the third year and that as long as there are no changes that I would be in the clear). Again, the pap smear was disappointing, and a third colposcopy was scheduled. (That was the procedure that was discussed above almost being rescheduled due to someone else’s c-section). This time, things had progressed from CIN1 to CIN2 and CIN3. She told me I would need surgery to remove pieces of my cervix to prevent the growth of cancer. Below you can see the Mayo Clinic’s diagram on what the cells on the inside and outside of the cervix look like with CIN1-CIN3 dysplasia compared with cancer.
I called my best friend, who had almost died of cancer at the age of 28 from exactly this same chain of events. She immediately gave me the name of her University of Chicago specialist and told me to call the office that day as her doctor had “saved her life and was the only person who had taken her concerns seriously”. She told me “Forget these podunk suburban baby-deliverers you need a researcher who is a leader in their field not someone who does this stuff just because they have to sometimes.” Unfortunately, her doctor couldn’t take me because he ONLY deals with people who already have cancer. However, his office called me back the SAME DAY, connected me with someone on that doctor’s team, and got me an appointment within 10 days for a second opinion. I had my medical records sent over to the new doctor’s office for him to review prior to the appointment. In the meantime, I researched him. He was an MD and has TWO PhD’s from Yale and countless awards. So, I was hoping that if anyone could give me good advice it would be him.
This man spent 45 minutes with me in his office (in a suit across his desk – not on a stool in some exam room). He gave me an entire science lesson on what was going on in my body. He showed me diagrams, answered all of my questions, and reviewed my case thoroughly. He actually knew my gynecologist and had gone to medical school with her father. He assured me that she was a competent doctor, but he had concerns about my case. He stated that each of the 3-years’ worth of biopsies that she’d taken were far too small to be conclusive or enlightening so that there is a “small chance” that I already have cancer. He concurred with the necessity of the surgery to remove the damaged tissue and find out if there was cancer already and prevent it if there wasn’t. When I told him that I had asked about the HPV vaccine 2-years prior he said “yes you absolutely should get it. It’s been found to boost the immune system in already infected people and help clear the infection. Any gynecologist who has been keeping up on their research should be recommending that since about 2016-2018. I’m surprised and disappointed you were told not to. We’ll get you that shot today before you leave today.” He assured me that my doctor was competent. I specifically said to him, “this is the only life I have. I don’t want competent, I want Gray’s Anatomy Christina Yang-style, confident brilliance. So, are you brilliant?”
He told me that he didn’t want to toot his own horn and I said, “please toot.” He told me he’d studied at the lab of the man who had invented the Pap smear and had invented a more modern version of doing this surgery that his hand-selected team trains on in practice labs and that he’s done thousands of them successfully. He told me that he’s just a doctor and not a magician and that he can’t help what’s already there but that he does have a plan for the best-case scenario, the medium-case scenario and the worst-case scenario for my care already in place with specialists that he trusts already on hand to assist. He sent me home with diagrams, information, and confidence. I didn’t leave his office wondering if he cared about me. And it wasn’t his “bedside manner” that converted me to switching to his office. He was very clinical. He wasn’t unkind or cold, just very business-like. His personality was actually a bit colder than the other doctor. But he was thorough and exuded scientific knowledge. And his office has a TEAM of specialists who deal with ONLY this issue. His office has both early and afternoon appointments and an entire day of the week dedicated to only surgeries and procedures. I left scared of the future but confident that I would get the best care that his office and team had to give.
So, when I had my surgery yesterday and he walked (more like swaggered) into the room beforehand he calmly explained the whole process to me. He assured me that if there was bad news, he would call me immediately, but he still believes that the chance is small, despite my previous doctor’s (in his words) “lack of attention to detail”. He gave me his cell phone number in case I didn’t feel well, (Despite it being the 4th of July weekend), or something felt wrong when I got home. He explained all of the aftercare instructions to my boyfriend and personally introduced me to all of the nurses on this team. He is not “in this just to hold new babies” and clearly keeps up with and even contributes to new research. I am grateful to have found him. Every interaction that I had with all of his staff have been caring, professional, and have made me felt like my health was their priority. I only wish that I had switched doctors earlier – but due to my having such a hard time finding doctors without months-long waits, I hadn’t even considered that I deserved better.
So today I sit and recover with my painkillers and heating pad – wondering if I have cancer or not – wondering if my first doctor’s lack of attention to me prevented me from catching this earlier. (No less on the 4th of July one year after the overturning of Roe v. Wade). I also sit worrying not only about myself but what will happen to other women when doctors are so swamped that they aren’t keeping up with the most current research, aren’t spending time with their patients, aren’t able to listen to them, and aren’t able to provide them with the care that they deserve. When to keep the lights on, private-practice doctors cram in as many patients as possible, don’t really listen or craft high-quality care plans, or just plain don’t prioritize women’s health beyond the run-of-the-mill normal pregnancy. I will say this much – we have to do better when caring for women in this country. People who can’t easily take time off of work but want to be healthy deserve the opportunity to do so. New moms, moms-to-be, never-moms, and moms-who-want-to-be all deserve high-quality specialty care not just “competence”. If they don’t get it, who will run stores, banks, schools, and retail shops? You want the world to keep on rolling? Supply chains to stay intact? Students to stay in classrooms? Businesses to run? Then we need healthy women who are able to access high-quality care when they need it without delays, under-prioritization, lack of insurance, or a lack of empathy. Women make up more than half of the population worldwide – it’s time to work smarter not harder and to just plain DO BETTER.